How "Consumer Reports" FDA Approvals Could Hurt Biosimilars

By Anna Rose Welch, Editorial & Community Director, Advancing RNA
It’s been an important couple of weeks for the FDA and biosimilars. Recently, Amgen’s adalimumab and Sandoz’s etanercept faced Advisory Committee (AdCom) meetings. Both candidates received unanimous votes to be recommended for approval. And though there have only been two previous FDA biosimilar approvals, these most recent AdComs indicate the FDA is growing more comfortable with reviewing biosimilars.
Naturally, this increasing willingness to approve and extrapolate biosimilars has been met with questions about why more attention isn’t being paid to accelerating their approval. John Carroll poses a great question in his ENDPOINTS article: “Where’s the outcry from Congress for speeding up their approvals?” After all, there has been a general push for quicker access to new cancer drugs. There are even several members of Congress in favor of approving Sarepta’s eteplirsen for Duchenne muscular dystrophy, even though it boasts data from only 12 patients.
Compared to the latter, especially, biosimilars are on much stronger footing. Based on their data packages, Amgen’s and Sandoz’s biosimilars were deemed highly similar and viable for extrapolation to all indications — both in their AdComs and their FDA briefings. They each presented switching data as well, suggesting that patients already on the biologic could make a single switch to the biosimilar.
Yet, there’s no congressional push to expedite biosimilar approval. Rather, there has been one recent proposal (not congressional) I’ve stumbled upon in The Wall Street Journal (WSJ) that suggests several changes to the FDA approval process. But instead of speeding up approvals, these suggestions could result in a much more tentative decision making process. And though these ideas have their merits, they pose some danger for biosimilars.
Why A Graded Approval Process Is Not For Biosimilars
In his column for The WSJ, John Sotos, medical director at Intel Corp, argues in favor of the FDA taking a “Consumer Reports approach” to new drug applications. Sotos writes that the current approach —“which copies Roman emperors who signaled a gladiator’s fate with either a thumbs-up or thumbs-down”— is not appropriate for pharmaceuticals today. He says, “The FDA would continue to review new drug submissions in its careful and scientifically demanding way, just as it does now, but instead of making an approve/don’t approve decision, it would issue a rating of the drug’s safety, efficacy, and the degree of evidence supporting safety and efficacy.”
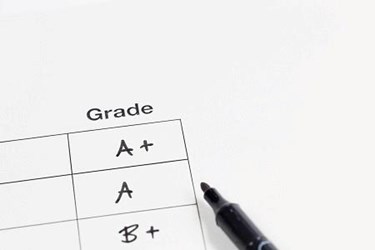
For example, he describes an experimental cancer drug that earns a B+ for efficacy against stage IV-A squamous cell lung cancer, an A for safety, and 2 out of 10 for degree of evidence. (In his proposal, he expects this process would allow drugmakers to submit clinical trial information in stages. As such, the degree of evidence score would ultimately increase as the manufacturer submitted further clinical evidence.) The goal here is to give doctors and patients other methods for determining the appropriate treatment. In addition, because submissions of clinical trial data would be on a “rolling” basis, drugs would be able to reach the market more quickly.
The concept of “breaking down” an FDA approval is not novel for the FDA. After all, many patient groups have proposed that FDA committees reviewing biosimilars should be able to vote yes or no for each indication. Allowing them to do so would eliminate any reservations about extrapolation. Similarly, a much-needed biosimilar, which has been proven effective in clinical trials for one or two indications, could be kept from market if voters had concerns about an untested indication.
I give Sotos props for this physician- and patient-centric approach to approving drugs. Using the “graded” approach would help patients better understand their physician’s prescribing decisions, and, in turn, be able to more actively participate in these decisions. For example, should a doctor decide to go with a medicine that was not the most highly ranked, the patient could better understand that decision as well. Preserving the doctor-patient relationship is a key concern patients have for those making biosimilar regulatory decisions.
There are, however, some elements that concern me when thinking about how Sotos’ process would apply to biosimilar approvals. One of the benefits to this strategy, Sotos argues, is that drugmakers would be driven to “compete on the degree of evidence supporting their drugs, not just their safety and efficacy. Thus, a pharmaceutical company could advance at least one component of a drug rating by performing more studies on the drug.”
Now, this could help address the dearth of post-marketing studies — which was a concern expressed regularly in both Amgen’s and Sandoz’s AdComs. I suppose this could also be a solution to concerns about extrapolation. Should the FDA ever charge committee members with the responsibility to vote yes or no based on indication, companies could perform and submit clinical trials data on the questionable indications for future addition to the label like any other biologic.
But the solution’s emphasis on more clinical trials makes me hesitant to accept Sotos’ proposal for biosimilar developers. (To be fair, his article is focused primarily on novel drugs. But any adjustment of the approval pathway would likely affect the way biosimilars are approved as well. In fact, I’m surprised he didn’t pay heed to how this kind of approval process would apply to biosimilars, given the rising interest in approving these treatments in the U.S.) Having to perform additional clinical trials not only defeats the purpose of the abbreviated biosimilar pathway, but creating grade levels and safety ratings could spur additional differentiators between a biosimilar and its reference product. (Not to mention, the process of putting together a rating system would likely cause some epic headaches.)
As the positive recommendations to extrapolate the U.S.’s third and fourth biosimilar drugs show, the FDA is doing what it can to ensure an abbreviated biosimilar pathway. Though there is still a general sense of uneasiness over extrapolation, more time and experience should lessen these insecurities. After all, we are following in the footsteps of the EU, which has already taken the extrapolation plunge. To date, these countries have not observed adverse effects in patients taking Remicade biosimilars for all of the indications. Even Health Canada, which originally rejected Inflectra for gastrointestinal indications, recently added these indications to its label. If we’re looking to cut the number of barriers to FDA biosimilar approval, I feel as though Sotos’ proposal would take biosimilars in the opposite direction.
